Background
Artificial intelligence (AI) is not new, but creative new projects are highlighting the adaptability and the broad utility of this technology. A recent entrant to the AI arena is RCM Brain, a startup that is focused on Revenue Cycle Management (RCM) for providers in the healthcare industry. Launched this past June, the RCM Brain solution is an AI-driven RCM rules engine and workflow automation platform built to help medical providers and third-party billing companies better manage healthcare claims processing. RCM software manages a range of functions associated with claims – including scrubbing Electronic Medical Records (EMR) systems with a bot called BETH – as it engages with data from across multiple legacy billing systems, claims data clearinghouses, and insurance (payer) platforms.
According to RCM Brain president and founder John Williamson, revenue cycle management is a complex process, which may involve coding the claims with right procedure and diagnosis code (there may be up to 150 pieces of information on a claim), submitting claims to right insurance company, assuring quality of the data input, accounts receivable, including managing claims denial or no response at all, and matching bank account records with what is being paid by the insurance company, what has been paid, and what is still owed – a “triage of information” that Williamson call ‘posting’. Depending on internal resources and operational policy, providers may choose to handle their own revenue management cycle – or outsource all or portions of it. As a result, RCM Brain works with a variety of organizations, ranging from healthcare providers, to third party claims processors, to data clearing houses, to various insurance payers. RCM Brain’s need to access and manage data in different formats, from multiple systems, for clients’ varying functional needs presents a level of complexity that is best managed with self-learning AI and robotic process automation.
Building the business
In startup mode for two years, RCM Brain began by building a minimally viable product that would require ongoing development and refinement. For example, at first the software could not read PDFs, but the company quickly learned that virtually every customer engagement going forward would likely involve PDF documents. The initial bot was immature – it was not capable of all the work needed to search for patients and update records. Similarly, the self-learning in the rules engine was not fully formed – it could work with rules created by RCM Brain staff, but could not machine learn new rules.

In addition, RCM Brain need to develop a product that could address the complexity presented by different customer environments. To illustrate, Williamson noted that while specific job functions (coding, submitting, accounts receivable) are largely the same, data is not always received in a format that is easily digestible. RCM Brain acquires data through three different methods. The BETH bot logs in with a given password to the billing module of a clients’ Electronic Medical Records System, and runs a report to scrape and export data on all patients that have submitted a claim. Or, EMR data may be delivered from a data clearing house, which has already cleansed the data. A third method relies on AI to extract data from scanned PDFs, which may by typed or handwritten. As Williamson explained, this third approach may involve manual intervention and hence is most labour intensive: in one client example, 15% of documents were unreadable by the machine, and another 20% were readable but a human quality assurance process was needed to monitor for errors. In extraction, “there is a percentage that is no touch, a percentage that is partial touch, and a percentage that is fully typed in by a human,” he added.
For RCM Brain, a key requirement is to take information from these disparate sources and standardize it for internal processing. Once information is mapped to the company’s data schema, machine learning is applied to help RCM Brain understand and address claims issues. For example, AI can be applied to discover what led to a claims denial when a certain set of procedures for a particular patient and/or provider were used, and then new rules built to tailor claims processing for certain circumstances or companies going forward. According to Williamson, this kind of predictive, AI-based process improvement can mean the difference between a claim being paid on first submission or not, and through application of improved procedure to the rules engine, help to advance development of the platform overall.
Accelerating go-to-market strategy with IB
To ease customer adoption, RCM Brain’s goal is to standardize so that an out of the box solution already has most of the rules needed for claims processing. Although much of the functionality in the solution may be generic, different customer software works differently. As a result, the company has learned it must customize the last mile to align with client environments. In addition, RCM Brain has engaged with customers that have custom reporting requirements. To balance work towards standardization against client’s custom needs, the company looked to connect with an outside provider of reporting and analytics capabilities. In the early stages of solution development, Williamson explained, the company’s engineering effort was highly focused on the core functionality of the bot and the rules engine, and hence RCM Brain did not have the time or the expertise needed to build out analytics capability in the platform. To quickly add this capability, RCM Brain chose to work with Information Builders (IB), a BI and analytics firm with a strong product portfolio, as well as deep domain knowledge and strong connections to RCM Brains’ key market – the healthcare sector.
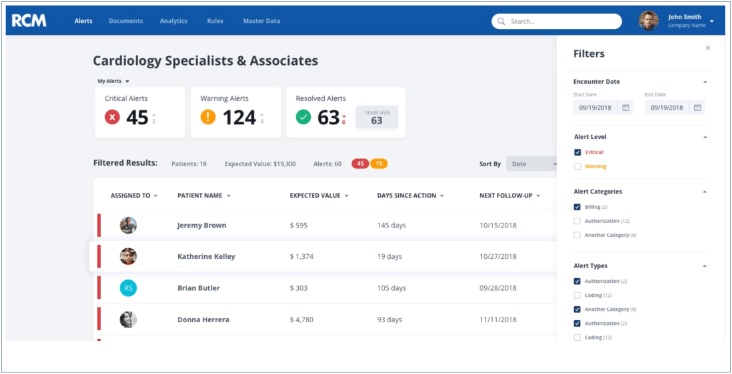
But Information Builders offered another partner advantage. RCM Brain wanted access to analytics capabilities for its own purposes – to monitor the operation of BETH, and to improve RCM workflows. IB’s WebFOCUS Portal could be deployed, for example, to build dashboards that would permit RCM staff to visualize and drill into claims data. Using dynamic charts that could provide insight into issues such as payment inaccuracies, staff could apply predictive analytics to improve automated processes. However, the company did not expect that every customer would have a similar need. In its business discussion with Information Builders, RCM Brain found the flexibility needed to enable a startup company with fewer resources and more singular focus on core software functionality, to offer interested clients a fuller complement of services. Williamson explained: “We needed to be able to invent in a clean way. We needed to make it so that not every customer would have to buy analytics, but that we could see the analytics of every customer. We are a startup – so we needed to structure our deal with Information Builders in a way that made sense. We came up with a plan that brought down the annual cost.”
Williamson described this plan as “almost pay as you go, a little closer to the SaaS model. The unique arrangement provides for RCM Brain to pay a modest fee for its internal use of IB analytics; but when customers want access, they are charged for the sale of analytics/reporting capability and an additional, fee is paid back to Information Buildings. He also described the arrangement as a “more fair” enabler of the small business. “Some companies can afford to pay a big annual fee up front,” he explained, “but there’s also this migration to payment plan structure where you pay as you use things. We’re kind of in the middle of those.”
Work with IB
For the customer, RCM Brain’s use of Information Builders analytics is transparent. “What the customer sees is not branded: it’s embedded, its’ kind of an iframe on a page with tabs. It just looks like part of the RCM platform. There’s only one log in; we do the log in passively behind the scenes,” Williamson explained.
Working with Information Builders was similarly straightforward, he added. During implementation, RCM Brain used some Information Builders services, but has since moved on to work with an IB SI partner, India-based Amtex, who has dedicated two engineers to the account. According to Williamson, these engineers work with no oversight from the US team, and communicate directly with RCM Brain a couple of times a week on changes and chart work might be needed: “It’s a lot more expensive for us to have that expertise in house than it is to have a partner that already knows how to use the tool. We have two people that cost less than one person in the US, and they both know how to use the tool better than we would. It’s far simpler, and more cost efficient.” Amtex support is delivered on WebFOCUS, as opposed to data science exploratory research, however, the partners work easily together to create an integrated solution for customers. Williamson explained, “Once we figure out how the data points work together, and what the math is, we will say put this in a chart that looks like this, and here are the requirements. This has been a far simpler approach for us than having to have people who know every nook and cranny of WebFOCUS.”
To speed reporting, RCM Brain has recently begun to use the Information Builders Hyperspace data store solution. The company has built its data warehouse on Mongo, but when WebFOCUS was implemented, RCM Brain discovered that this store was less responsive to queries – that the analytics ran more slowly. To solve for this issue, RCM Brain now “takes a snapshot of that [data], and shifts it over to the Hyperspace database format that Information Builders often uses. We’re creating a reporting layer within the Hyperspace – where we take from our data schema, which is pretty split up, flatten it out, and bring it into the Hyperspace.” This allows the report to load a lot more quickly. Williamson estimates reporting may be up to three to four times as fast as with Mongo alone. “We put a lot of effort into making other areas of our solution pretty responsive to suit people’s expectations, so we couldn’t have customers sit when they got to the analytics area. We couldn’t have them wait while the data loaded…”
Value prop for customers
Describing RCM Brain’s main value proposition for customers, Williamson pointed to the solution’s ability to reduce labour costs, remove tedious work, and to eliminate errors associated with manual processes. “Revenue cycle work is tedious and complex, with millions of coders and billers devoted to these activities for both providers and payers,” Williamson noted, and despite this investment of time and money, revenue leakage of 5 to 11 percent due to underpayments continues to occur on an annual basis in the US healthcare system. But by using RCM Brain services, customers can begin to turn this around. In the case of the RCM posting services module – where money comes in from the insurance payer, and has to be matched up with the money that has come in from the patient in a bank statement – Williamson estimates that labour in this process can be reduced by 60-80 percent through use of the bot. “For every 5,000 claims a provider would send out, there would be two people doing that job. If you have 50,000 claims a month, you would need a small army of 20 doing the posting. But with RCM Brain, now you can reduce that to four.”
Value prop for RCM Brain
In addition to the ROI benefits this automation can deliver to clients, working with Information Builders allows RCM Brain to offer additional functionality. Williamson cited the example of one customer that is in the business of acquisitions, which has information in multiple systems with very different reporting options. This variation makes it hard for the company to consistently compare data; however, using a combination of RCM and IB technologies, RCM Brain was able to ingest all data, and provide the customer with a single view of the data that is based on the client’s own performance metrics. Success with this customer depended on speed – RCM Brain was able to provide a unified view with custom reporting within 30 days of implementation start.
This kind of success story is critical to a startup organization, which needs to quickly demonstrate value in order to gain market traction. According to Williamson, “If we can start to see those kind of results, where we can give the client visualization and data access – maybe even as the fastest part of the implementation – that’s a big win for us.”
Working with Information Builders, RCM Brain has been able to provide an additional level of service, and respond quickly to customer need for customization, while demonstrating its ability to stay on top of BI and analytics – without reinventing the wheel. Williamson described RCM Brain’s core functionality – building capabilities that work with many systems, the self learning rules that go into AI, and ensuring scalability as “a big lift.” But by embedding analytics capabilities with “instant appeal” while building out more challenging solution components, he believes that its possible to raise the RCM Brain profile. Through work with IB, the company has been able to address customer preferences for engaging with a single vendor for multiple capabilities; “IB rounds out our offering,” Williamson explained. “If you brought a solution to market that didn’t have analytics and reporting, it would be an obvious deficiency – we’re plugging a hole that otherwise we would have had a harder time plugging.” The Information Builders partnership has delivered cost saving to the client, marketing benefit to RCM Brain, and productivity benefits to both company and client.








