The challenge:

Markham Stouffville Hospital (MSH) is a two-site community hospital that delivers diagnostic services and clinical programs in acute care medicine and surgery, addictions and mental health and maternal and child rehab/transitional care out of facilities located in Markham and Uxbridge, Ontario. With other specialist providers, the hospital’s 450 physicians, 17 midwives, and 1,900 staff service the community care needs of almost 400,000 residents of Markham, Stouffville and Uxbridge.
In planning for its future, MSH is working to address the region’s high population growth through initiatives aimed at increasing hospital efficiency. As May Chang, EVP and Chief Administrative Officer at MSH explained, “we know that our population is going to grow and that we need to become much more efficient so that we can expand our services to meet new demand. We are not going to get a lot more money from the government so we have to be very resourceful in how we accommodate our growth – from a public perspective, people expect that of us. They want us to use our resources wisely, and we’re trying to figure out how to increase our efficiency so that we can put back more into clinical care.”

Two years back, this commitment to performance led MSH to establish an Office of Innovation whose mandate is to support initiatives that will increase operational efficiency, but also help the hospital to improve patient experience and patient outcomes. With these two objectives in mind, staff, and even patients at the hospital, have embarked on specific projects, which in turn have inspired new appetite for additional means to improve service delivery. “We have been able to create a culture of innovation in the hospital,” Chang explained, through a variety of activities, including innovation fairs: “we didn’t know what to expect, but the turnout was amazing. Staff came in to review the showcase projects, and asked management to do more of this, as they now also have some ideas to contribute.” From one or two ideas at its inception, the Office of Innovation now supports 15 to 20 projects, including initiatives undertaken in partnership with universities, ventureLAB, MaRS, and even with the City of Markham.
As in the healthcare industry generally, technology serves as an important enabler of innovation at MSH. According to Richard Opara, Director of Planning and Business Intelligence at MSH, “change in healthcare in Ontario is now very rapid. In the last five years, there has been more change than there was in the previous 30 years. We think the hospitals that are going to survive in this environment are those who are able to learn fast.” For MSH, a key input to “learning fast” is information on current performance, the benchmark against which future targets for improvement can be set; however, providing ready access to that information has proved challenging. Chang described this issue as one of data management. “Hospitals collect a ton of data. But trying to take that data and turn it into useful information is very difficult,” she explained. “It can be a very manual process: we spent a lot of time collecting and pulling data, but very little time actually doing the analysis needed to take that information and improve our patient experience, improve the quality of care that we provide to our patients, or to look at how we can create efficiencies in our own operations. We thought there has to be a better way, and we’re now looking at ideas around ‘smart care’. How do we provide care in a way that is much smarter than we have historically?”
The response:
In answer to Chang’s question, MHS opted to deploy technology that would speed staff access to actionable information. A new business intelligence tool, which Opara identified as a critical piece of the hospital’s innovation portfolio, would allow the hospital “to learn quickly from data collected about patients, take that learning and deploy it literally the next day in the form of actions that would improve the experience of the next patient. A four phase initiative undertaken through implementation of Information Builders’ WebFOCUS platform, the MSH project launched with delivery of business intelligence to improve clinical care. Specific information that the hospital looked to derive from clinical data sets revolved around quality metrics that would be serve as performance benchmarks, and as the basis of process improvement going forward. As Chang explained, “we wanted information from the clinical data set to answer questions like ‘How are we doing with quality?’ ‘What are some of the measures that we would like to see to help us improve process?’” In addition, MSH aimed to quickly deliver data that physicians and clinicians could use on a daily basis. One hospital goal, for example, was to assess readmission rates, an important provincial indicator that is used to measure service quality, and improve that by five percent each year.
Implementation:

Opara outlined a three stage process for the BI implementation, which encompassed tech deployment but also measures to ensure successful uptake of WebFOCUS capabilities. The first step involved identifying customer requirements. In this “most important phase,” the hospital invited representatives from all key stakeholder groups, including physicians, frontline nurses and clinical managers, to provide their input in a series of half day sessions. Stakeholders were asked: “What information do you use; what are your key pain points, what type of insights would help you get things done faster, cheaper and with better patient care?” A second step involved mapping customer requirements to the data, a task that the database team managed, to ensure that the data needed to answer stakeholder questions was in fact available. A final phase involved actually reaching back to into hospital databases to pull the data. According to Opara, the eight person BI project team, consisting of two database administrators, four Information Builders support people (technical and front end resources), three representatives from the hospital’s ‘business’ units, and the project manager (Opara), developed a long list of possible requirements, but to keep the project manageable at the outset, scoped the top five most important areas and built the first set of dashboards around these.
In contrast to other, larger facilities which may operate 20 – 30 different information systems, MSH benefited during implementation from having a single, integrated EHR (Electronic Health Record) system. All departments – Emergency, Lab, Diagnostics, etc. at the hospital use MEDITECH modules that form part of an integrated application. According to Opara, having all patient data in one system made extraction of data to feed into the BI tool a much simpler proposition. Other data did require integration. For example, data from the Med 20-20 coding database (Med 20-20 is a health information management solution for data transformation) had to be pulled and transformed using ETL tools. This was accomplished through two means: the Information Builders solution package came with some advanced integration capabilities, including iWay Migrator adapters designed to connect two data sets, and which enabled coding data to connect to the hospital’s primary SQL data source. But for proprietary processing of hospital data – the matching and the cleansing – MSH DBAs wrote ETL programs to support the daily extraction and transformation of data, and for checking the quality and validity of the data before storage in the SQL data warehouse, the repository from which reports are read. Applied to the data every day, this logic was based on a vision of the kinds of dashboards the hospital wished to create.
The dashboards themselves were designed to communicate a lot of information in the simplest way possible in order to produce an intuitive user experience. After trying a number of options, the BI team settled on an approach that uses a lot of simple colours to identify exceptions. For example, the screen of the Emergency Department (ED) dashboard shows eight boxes, each representing a key performance metric that is marked with different colours, based on relative achievement of a pre-set reference benchmark. “So green is good; yellow means I need to pay attention,” Opara explained, and to address a yellow alert, the user can drill down to access more detailed data. For case costing reporting and analysis, the next phase of the BI implementation, the team intends to develop a different approach that will accommodate the additional financial information that would be part of this data set. “The look and feel of the Fitbit app,” is the design principle Opara is looking for, with a short summary and individual widgets with just the right amount of information that can generate more as the user hovers over the box. “That way, you are presenting information with a certain cadence. You can go as deep as you want, or at a glance, see what’s important. We are really trying hard to minimize the training effort. We want it to be as intuitive to front line staff as it is to senior execs.” Content for the dashboards is organized according to business focus, with data reporting for financial, patient, strategy and operational insight, and though role-based dashboards have not yet been developed, rules-based access, depending on security ID, is in place so that if a doctor or a nurse logs in, they see different data.
All told, MSH’s three stage implementation process took approximately three months, an accelerated pace that compares favourably with deployment times in other institutions. Chang added, “we’ve been told that our ability to deploy was much faster than most organizations. People told us they were fascinated by how quickly we were able to get that quality data because it’s taking others over a year to do the same.”
Lessons learned:
The relative ease with which the hospital was able to manage the technical aspects of the WebFOCUS deployment meant that the most critical aspect of the BI project was understanding what the vital questions were, and what pieces of insight should be fed to physicians, clinical executives and frontline workers in what way to help them become more effective. And the team spent a good deal of time at the beginning of the project trying to identify the right questions. But this focus also served to engage staff in the project: as Chang noted, the goal was not simply to provide information, but rather to “actually use that data to help push a metric that we are trying to improve on.”
As the hospital moves to the next stages of its BI rollout, encompassing advanced reporting for case costing, financial and HR data, the team intends to apply learnings around stakeholder engagement, specifically, the need to identify concrete ways that the BI solution can provide specific benefits. As Chang explained, “In all my years in healthcare, I have found that the most important thing you have to get is clinical buy in. Without this buy in, you can try to make any system work, but if the clinical folks don’t buy in, they won’t help you. So engagement of physicians and clinical frontline staff is really key to the project.” To encourage this participation, MSH launched its BI project with clinical data, assuming that buy in would follow for the case costing phase once staff were able to see the value in the clinical quality data set.

As an example of this kind of concrete benefit, Opara described a reporting initiative within ED, shaped by Dr. Andrew Arcand, Chief of the Department of Emergency Medicine, “one of the more digitally savvy doctors who is a champion of using data to solve patient care problems.” As the entry point to a hospital, ED is often a bell weather for patient care in other areas. According to Opara, one big issue is the fact that patients may come into ED, but leave without being seen, and there is a “percentage left without being seen” metric that tracks how the hospital is performing in this critical process. Using the BI dashboard, Dr. Arcand has been able to identify a correlation between the average amount of time it takes for a physician to see an ED patient on a given day and the percentage of patients that leave without being seen. The intended outcome of this analysis is reduction in the “left without being seen” number, through improvement of physician time to respond. To support this initiative, the BI tool will provide physician time assessment at the individual level – by day and by case – in pretty much real time. Prior to the BI implementation, this performance data was available; however, Dr. Arcand was provided with aggregated numbers, maybe on a monthly basis, that wouldn’t tell him where to look to improve ED response.
In the next phase of the BI project, the MSH team expects use of the tool will increase significantly with roll out the case costing data. As Chang explained, “There’s a lot of focus in healthcare on efficiency, and doctors are really competitive – they want to be seen to be providing quality, efficient care. Case costing data will allow individual physicians to see “how is my care ranking against that of my peers?” But in an effort to ease acculturation of care groups, the team has taken some steps from a sensitivity perspective to help physicians transition to advanced reporting at an acceptable pace. For example, since some individuals initially may not be comfortable with such fine-tuned analysis of their performance, for now the BI dashboard does not identify individual physicians by name: code numbers have been used instead that will allow a doctor to see performance on their own cases, but not that of their colleagues, and that will allow them to benchmark against the average. Once physicians are more accustomed to the system, they may be more comfortable unblinding the data. Chang added “physicians will look at the data and see that someone else was better, and begin to ask questions. They know where they stand, and will try and make the kinds of improvements needed to put them at the top. We’re not pushing them to do it, but the data is powerful enough that it pulls them into quality improvement.”
Outcomes:
Assessing the WebFOCUS deployment, Chang was pleased to report significant progress on the primary implementation goal: “We have been able to take the information that we gather and turned it around; so instead of spending 80 percent of our time finding the data and 20 percent analyzing, we have flipped it. We now spend 20 percent of our time getting the data and 80 percent of the time doing the analysis that allows us to truly figure out what we are doing, how we can improve our service, and how we can improve quality of care.”
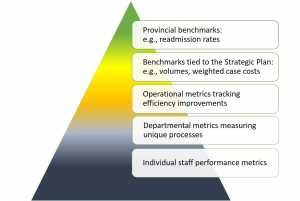 A data driven process, this analysis has been built on measuring the relative achievement of healthcare benchmarks that exist to help the province and individual hospitals assess performance, and set targets for overachievement of key performance indicators. With BI in place, MSH is now empowered with the information needed to address a pyramid of benchmark targets. At the top level, provincial benchmarking of items such as readmission rates that the hospital is mandated to report on help MSH to understand how the institution is performing as a whole and relative to other facilities. At a second level, MSH has put in place benchmarks that are tied to achievement of its Strategic Plan – metrics that Chang explained are intended to “push the needle, for example, lower our cost of weighted case so we can invest in our future, better understand our volumes, whether or not we are providing the right services, and where are our patients coming from.” Metrics exist at a third level to ensure that efficiency improvements in hospital operations are moving as they should; at a fourth level, specific departments will have their own metrics to measure performance for unique processes; and at the base of the pyramid are individual staff performance metrics.
A data driven process, this analysis has been built on measuring the relative achievement of healthcare benchmarks that exist to help the province and individual hospitals assess performance, and set targets for overachievement of key performance indicators. With BI in place, MSH is now empowered with the information needed to address a pyramid of benchmark targets. At the top level, provincial benchmarking of items such as readmission rates that the hospital is mandated to report on help MSH to understand how the institution is performing as a whole and relative to other facilities. At a second level, MSH has put in place benchmarks that are tied to achievement of its Strategic Plan – metrics that Chang explained are intended to “push the needle, for example, lower our cost of weighted case so we can invest in our future, better understand our volumes, whether or not we are providing the right services, and where are our patients coming from.” Metrics exist at a third level to ensure that efficiency improvements in hospital operations are moving as they should; at a fourth level, specific departments will have their own metrics to measure performance for unique processes; and at the base of the pyramid are individual staff performance metrics.
According to Opara, the business intelligence initiative is helping MSH to integrate data and metrics across these various levels, and to support the filtering down of goals outlined in the MSH Strategic Plan or provincial strategy. Ultimately there are two key metrics that apply at the first and second levels – the hospital’s cost per weighted case, and its readmission rate. But building up to the clinical and cost reports are metrics that can be used, evaluated and socialized through BI at the lowest level; metrics taken at the patient level that can then cascade up by department, by program, by diagnosis, or by physician group “so that at any point we know where we are in terms of our cost and our quality.”
With BI insight delivered at each level, MSH can build a view of progress towards each of its benchmarking targets. But more importantly, Opara noted, “by creating that level of attribution, almost at the self-service level, we think it’s going to drive a new way of thinking. If I am a clinical manager, in charge of mental health, I might want to see how I’m connected to our strategy. There are certain reports in the BI tool that can show me the contribution of mental health to reducing the hospital’s two key metrics.” If an important exercise in technology deployment is to change culture to encourage exploitation of tools, at MSH, the team has also used the BI platform itself to mobilize workers to become invested in the achievement of broader goals. “We want people to be able to identify their role in helping us achieve our strategy,” Chang concluded.








